The potential of autoantibodies in the early detection of cancer: a podcast with Joseph Miseirvitch
Meet the speaker:
 Joseph Miseirvitch – Field Applications Scientist, Sengenics (MA, USA)
Joseph Miseirvitch – Field Applications Scientist, Sengenics (MA, USA)
Joseph Miseirvitch is a scientist with a passion for solving the unknowns in cellular, molecular, and biological pathways with over 10 years of experience in the life sciences. He is currently the Field Application Scientist for Sengenics covering North America. Sengenics is a precision medicine company founded in the desire to improve patient outcomes based on physiologically relevant, data-guided, decision making. Our platform enables the discovery and validation of autoantibody biomarker signatures for patient stratification, drug response prediction and development of companion diagnostics.
Transcript:
Jade Parker (JP): Hello, and welcome to OC talks, a podcast series exploring the latest advancements in oncology. I’m your host, Jade Parker, Oncology Central’s Senior Editor. In this episode, supported by Sengenics, we will be exploring the importance of autoantibodies in the development of cancer as well as how they can be used in the early detection of tumors. Joining me for this episode is Field Application Scientist Joseph Miseirvitch from Sengenics, a precision medicine company working to improve patient outcomes for physiologically relevant, data-guided decision making. Thank you for joining us today, Joey. To kick things off, could you please introduce yourself and provide a brief overview of your career to date?
Joseph Miseirvitch (JM): Sure. As mentioned before, I am currently a Field Application Scientist at Sengenics. My background is in cellular pathways with a focus in T-cell immuno oncology. I spent the last 4 years as a Field Application Scientist and prior to that I worked at the bench in biopharma and academia for 15 years before transitioning to a technical support role. I really enjoy what I do because it has afforded me the ability to not be narrowed by one particular corporate approach to immunology, but a broad spectrum of how many scientists and entities are individually approaching the research and progression of our understanding and ultimately our ability to heal people.
Thank you, Joey. So for our first question, what role do autoantibodies play in cancer progression and metastasis?
JM: Yes, good question. It has been documented that autoantibodies can play a role in cancer progression, specifically breast cancer. B-cells through selectively promoted lymph node metastasis produces pathogenic IgG, that targets HSPA4, which results in activation of CRC NF- kappa- beta pathway in tumor cells, so on, so forth all the technical stuff, and this ends up leading to mediated metastasis. Another example would be in ovarian cancer with CD20, positive B-cell suppressed tumor growth. But regulatory B-cells or Bregs induce immunosuppressive effects, which support tumor growth.
In addition, those with underlying autoimmune conditions such as rheumatoid arthritis, systemic lupus erythematosus (SLE), Sjogren’s etc., tend to have an increase in the probability of developing some types of cancer. While we often view autoantibodies as the means by which the body tries to fight off diseased states, there are some occurrences where they can be detrimental to our health. So, by improving our understanding of autoantibodies, we can develop therapeutics that can perhaps suppress some of these potential targets for cancer treatment intervention.
What are some of the advantages of using autoantibody markers over the traditional biomarkers, for example, protein and genomic markers?
JM: Traditional biomarkers are not better or worse per se when compared to using autoantibodies. In fact, it can be argued that genomic protein and autoantibody biomarkers together paint a clearer picture for diagnosis and treatment than each one individually. However, each do have their advantages and disadvantages. For example, we are finding autoantibodies give a much clear picture that outperforms proteins due to higher specificity and sensitivity.
Autoantibody biomarkers can outperform genomics mainly on cost but can also take into consideration environmental exposure. For example, chemicals inside the body, in real time and in response of systems and people who encounter certain environmental factors. So, again, just to reiterate, it is a multi-omics approach and I think all three really do have a role, but it all depends upon what the researcher is ultimately looking to gain knowledge of.
How can autoantibodies be used for the early detection of cancers and aid patient stratification?
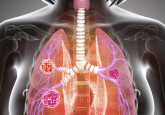
JM: There are several ways in which autoantibodies play a crucial role in our understanding and diagnosis of cancer. First and foremost, the moment the body detects a foreign entity be it a mutated cell or internal anomaly or an invasion into the body our immune system begins the task of combating the threat to the body. As a result, B-cells begin to produce tumor-associated autoantibodies. And in fact, these serum immunobiomarkers have already been detected in a range of cancer types before the onset of clinical systems.
Autoantibodies can be used as a diagnostic marker to aid in the early detection of high-risk populations. In addition to this, we can study autoantibodies from the perspective of a mechanistic approach. By knowing and understanding how antibodies alter cellular processes, we can better understand how to adapt or aid our immune system to be better equipped to fight metastases. Lastly, autoantibodies are produced in conjunction with antigens better expressed on the cell surface of cells that have gone rogue. In this way, we can use autoantibodies to develop targeted therapeutics that are highly specific to only the cancer cells without the onset of off-target results within the treatment regime.
Thank you, Joey. In which ways can tumor-associated antibody tests enrich cancer screening?
JM: Simply put, autoantibodies are the body’s first – and immediate response to really any changes, immunologically speaking that the body is addressing. Because of this, we can detect, long before symptoms arise, the presence of cancerous cells within the body. However, it really goes beyond this, because not only can we use autoantibodies to detect, but also we can use them to test for the effectiveness of treatments.
By kinetically analyzing the body’s autoantibody profile, we can see that in patients undergoing chemo treatments, a new emergence of autoantibodies that reflect whether or not the patient is reacting positively or negatively to the treatment regime. And to add to that point, we can further determine if successful remission was attained. So this gives us the ability to really tackle cancer in a truly offensive manner rather than from a defensive position.
Looking forward, how would you like the field to advance, say, in the next 5 years?
JM: Honestly, I think the realization that autoantibodies are the key to unmasking much of what we do not understand here. The ability to have a tool that provides you with accurate information about the state of any individual patient will translate to individual patient-centric care. So imagine if at a young age you go into your PCP and by taking a simple blood sample, you would know whether or not you have any number of autoimmune diseases, cancer, or really if your body is having any type of autoimmune response. Treatment can begin long before symptoms develop, and quite possibly, cure many people long before diseased state progresses to a point of no return. So hopefully soon we can start to develop cures to ailments vs blanket approaches, that are only nominally effective and in being able to detect at an early stage, we can actually even help to reduce the cost of insurance. For many individuals in the US, and perhaps, even worldwide.
JP: Thank you so much, Joey. To our audience, if you would like to find out more about precision medicine and autoantibodies, then make sure to head to www.sengenics.com or follow the links in the description below. Thank you so much, Joey, for your time in taking to talk to us.
JM: Thank you for having us.
JP: It has been absolutely great to see where the field is heading and how precision medicine and autoantibodies can tie into and really push forward on early detection and giving those personalized treatment options.
If you’ve enjoyed this episode, to all our listeners, I would like to find more like them, then make sure to head to www.oncology-central.com. You can also follow us Twitter for regular updates on the latest news and opinions in the field. So, thank you again, Joey, for joining us. Thank you to all of our listeners.
In association with:
The opinions expressed in this interview are those of the author and do not necessarily reflect the views of Oncology Central or Future Science Group.