Using 40-GEP to enhance metastatic risk assessments in cutaneous squamous cell carcinoma
Meet the speaker:
 Sherrif Ibrahim – Assistant Professor in the Department of Dermatology, University of Rochester Medical Center (NY, USA)
Sherrif Ibrahim – Assistant Professor in the Department of Dermatology, University of Rochester Medical Center (NY, USA)
Dr Ibrahim is an Assistant Professor in the Department of Dermatology at the University of Rochester Medical Center. He completed his dermatology training at the University of Rochester and a fellowship in skin cancer surgery, laser surgery, and cosmetic dermatology at the University of California, San Francisco. His practice is focused on procedural and surgical dermatology including the management of skin cancer with Mohs surgery.
Transcript:
Could you give our listeners a brief introduction to cutaneous squamous cell carcinoma and the current risk stratification methods for the disease.
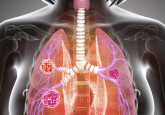
Cutaneous squamous cell carcinoma (cSCC) is the second most common skin cancer that we’re seeing after basal cell cancer and like other forms of UV-related cancers, are exponentially on the rise. If we look at disease-related mortality for SCC, we’re seeing an increasing trend of deaths related to SCC outpacing those from melanoma. In our field of dermatology, we’re used to saying that melanoma is the deadliest skin cancer and that might be true from the percentage of cases that go on to a bad outcome, but because the overall number of SCC is so much higher, we do see an overall mortality that is higher even though the mortality rate might be lower.
Currently, we are doing our best to stratify risk for SCC to see which of these cancers might go on to be metastatic or other poor outcome down the road. There are three risk stratification systems or staging systems that are in existence, of which two, the AJCC 8, and the Brigham and Women’s Hospital staging system are being used. Both of them rely on clinical pathologic features of the cancers such as the tumor size, the degree of differentiation – for instance in the Brigham and Women’s Hospital system if the tumor is poorly differentiated or if they have perineural invasions we can use things of those nature to stratify risk and do our best. I think those are the two main systems that we’re using now.
What would you say are some of the limitations of the metastatic risk assessments currently used for staging cutaneous squamous cell carcinoma in the clinic?
If we look at the performance of clinical pathologic risk factors alone, we see that about one-third of patients with metastatic disease were classified as being low risk, so having no high-risk features. The converse of that is that up to 75% of those patients who are classified as being high risk for metastases do not go on to have an event. Therefore, we still don’t really even know what the overall metastatic rate is for SCCs. I think if you look across cohorts from all the big studies that have been done, our best estimate is somewhere around 6% or less than 6% of all of these tumors spread, but because so many of these cancers do display some number of high risk features and therefore are classified as being ‘high risk’, we’re definitely over categorizing a large number of these tumors as being high risk and then missing about a third of the tumors that we’re classifying as low risks that do go on to have metastatic spread. Clearly, we’ve made some advancements in clinical pathologic risk factors alone and the current staging systems and the newest versions of these staging systems, but we can definitely do better.
You have had a recent publication in Future Oncology, investigating the use of the 40 gene expression profile tests for enhancing these risk assessments in the disease. Could you tell us a bit more about this paper please?
Our paper further expands upon a recent study that we published in the Journal of the American Academy of Dermatology about a year ago, introducing a 40 gene panel in conjunction with the people at Castle Biosciences (TX, USA) to be able to determine an independent biologic risk for metastatic spread. This is intended to use on a population of tumors that are already classified as being high risk by the presence of as little as one high risk feature. Then these tumors undergo gene expression profiling with 40 genes of interest from the original primary tumor using an RT-PCR technique. Then applying a validated neural network algorithm to classify patients as either having a low, moderate or high biological risk score they get assigned a class – class I being low risk, class IIA being moderate risk or class IIB being high biological risk. When taken in conjunction with the clinical pathologic risk factors, we can start to gain information that really further elucidates a patient’s likelihood of metastatic spread. If a patient is classified as being class I, they have less than half the risk of metastatic spread. If we look at a patient with a class IIA, they have about the same risk as some of the very high-risk features and if they have class IIB, it’s over a 50% chance of having a metastatic event. It really does help us come to a conclusion on an individual level of likelihood for metastatic spread.
How do you think that this test could help to overcome some of the limitations that you mentioned previously?
I think it’s really going to enhance our ability to refine staging and the predictability of metastatic risk for a given tumor. We see so many tumors in our practice and we see many SCCs per day in my clinic and essentially, all of them are high risk cancers. So it becomes very challenging to understand what to do with these patients. Do we send all of them for imaging? Do we send them for adjuvant radiation? Clearly, not all of these patients need that; like we mentioned before, 75% of the tumors that we classify as being high risk might not actually be high risk in the sense they don’t go on to metastasis. This is going to be a tool that we hope with further validation, could potentially become the standard of care and risk assessment for SCC.
What are the next steps incorporating the tests into clinical practice, and what would this mean for patients living with the disease?
The next steps for incorporating this into clinical practice is further validation. There is no question that this is something new and we’re using it right now in conjunction with clinical pathologic staging. We’re not yet ready to say we’re not implying to change anything with standard of care at this time, but when it comes to the management of high-risk SCC, there really is no standard of care. There are no set protocols for even anything as simple as frequency of clinical surveillance and follow-up for imaging for sentinel lymph node biopsies, and for those patients who might benefit from adjuvant treatments such as potentially systemic immunotherapy or radiation treatment. I think the initial next step in those studies are underway, which include further validation of the 40 GEP test and generation of lots of data. Then we do studies and once it’s validated, this becomes a springboard for numerous clinical trials downstream, because once we do identify those patients that are at significantly higher risk for metastasis of those class IIA and class IIB patients, the first steps will be increased surveillance, and that might just be seeing them more frequently in the clinic. It might be doing more regular imaging, whether it’s ultrasound or CT scans or MRIs or PET scans, and then eventually clinical trials with interventions such as additional adjuvant treatments in a hope to bring down the risk or the rates of metastasis in these very high-risk patients. On the flip side, it helps when the patients who are potentially lower risk, we do know that a large number of those will go on to metastatic spread. It helps us ease off the gas a little bit potentially in those patients who are deemed to be high risk by clinical pathologic staging, but yet have a low Castle class. Maybe we don’t do such high intensity follow-up and treatment afterwards. Those tumors that might be lower risk by clinical pathologic staging, but higher risk by Castle class score on the GEP test, perhaps we increase the intensity of surveillance, plus or minus intervention. So overall, of course, we want to bring down mortality from the disease; that’s our ultimate goal.
Do you have any closing comments you’d like to make?
Just that it’s an exciting time in medicine, we can see other precedents in diseases such as breast cancer where predicting biologic risk on an individual basis has really become standard of care. We’ve seen Castle’s earlier work with melanoma that is quickly becoming standard of care with that disease. And now the most recent addition to that list is SCC, as we further validate this test and learn how to incorporate it into our practice. And like I said, ultimately, learn more about this disease, develop better treatment protocols and standardization of those protocols across multiple sites, and hoping that our patients do better overall.
The opinions expressed in this interview are those of the speakers and do not necessarily reflect the views of Oncology Central or Future Science Group.