OCTalks: monitoring MRD in hematological malignancy management
In this interview we speak with Stacey Grieve (University of New Brunswick, Canada) and Keith Brunt (Dalhousie University, Canada) to find out what minimal residual disease (MRD) is and how it is currently monitored. Grieve and Brunt also explain their recent research published in the journal Nanomedicine, which investigates a novel tool to monitor hematological malignancies.
You can also view an animated video that explores the paper titled ‘Nanoparticle surface-enhanced Raman spectroscopy as a tool to monitor hematological malignancy’ by clicking here >>>.
Could you give our listeners a brief introduction to MRD in hematological malignancies and how MRD is currently monitored?
Stacey Grieve (SG): MRD refers to the cancer cells that remain in the body after someone is treated for their cancer. We are interested in monitoring and being able to detect MRD because it is these cancer cells that are responsible for the recurrence or the relapse of someone’s cancer. In general, we want the most sensitive and the most specific techniques to monitor MRD and for multiple myeloma the gold standard is monitoring serum immunoglobulins, which is a relatively invasive procedure for the patients. Some of the other approaches that we use, which are a little bit more sensitive, are things like next-generation sequencing or multiparametric flow cytometry. These come with significant cost burden and they also rely on a very specific understanding of the characteristics that make up each disease.
Please could expand on some of the current limitations of how MRD is monitored?
SG: It is about the sensitivity and specificity, and the cost as well as the burden on the patient. As I said for multiple myeloma, we use serum immunoglobulins, which are measured from the bone marrow. This requires patients to undergo a relatively uncomfortable bone marrow aspiration, which is an invasive procedure where we stick a very large needle into someone’s bone to extract the bone marrow. One limitation is how we can get the material that we need to monitor MRD and other limitations are about cost. Next-generation sequencing and flow cytometry come at large costs and are not always specific or they require certain presence of the disease to be able to detect any MRD.
Could you tell us about your recent research published in Nanomedicine investigating a novel tool to monitor hematological malignancies?
Read the Nanomedicine paper here >>>
Keith Brunt (KB): I think Dr Stacey Grieve did a great job introducing the problems that we face, particularly from a patient perspective but also from an institutional and clinical viewpoint. What we were really intrigued by was sort of that intersectionality of trying to improve our thinking about research studies in general. This is a highly collaborative work that we have completed, involving engineers and computer scientists, oncologists, microbiologists and medical translationists, what we were trying to do was address many of those problems that Stacey outlined.
It was looking at everything at once, rather than one specific thing. Rather than looking at just the cancer cells themselves, which you can imagine being a patient, having a large needle shoved into your bone or constantly going for blood work is painful and uncomfortable, and removing some of the uncertainty in having the limits of just say, one immunoglobulin profile, you are just looking at a few proteins. Instead, what if we looked at the entire biochemistry of the patient in one go?
View the video abstract for the journal article here
That is really what this paper was about. It was looking at what we call chemical or biochemical fingerprint using Raman’s spectroscopy and what we tried to do was augment the reference profiles that give us a sense of what is normal in somebody who is ill and older as well as a population that would be very healthy and young. In that way, we could identify the sensitivity and the specificity in the hematological malignancies that we were studying and try to address some of those problems. To tailor the identification of whether somebody needs treatment or is regressing with their disease and needs to be made aware of it in a way that they could ultimately improve their quality of life so that they could essentially live with cancer a bit better.
Those were the main objectives as it were and what you will see in the paper is a look at the machine learning algorithms that were used instead of humans, which were biased and were simple-brained creatures. But computers are beautiful. They can look at all these multi variables at once and then create network abilities to piece them together into principal components that matter to the clinical outcome for the patient. That is what this paper is about, building those really solid reference criteria and then adapting those computers to look in a more powerful way than a human could at many things changing at once.
How would you describe the process that you undertook to undertake the research in order to publish this paper?
KB: In simple terms, we collected plasma samples from various patients, those with cancer – hematological malignancies specifically – but also plasma from healthy young patients and people who are sick and in hospital for a different reason related to cardiac surgery. We basically said, how do we look, in an unbiased way, using machine learning algorithms that take the human equation out of it, at all the different variables that are in play in that plasma, using Raman Nano-enhanced signalling, and then link that to their clinical charts?
In doing so, we were able to find that it is very easy to separate the young, the healthy from those who are sick, but it is a little bit harder to separate sick from sick. Within the hematological malignancies, in those with cancer, we found some real salient bits that sort of show us that we can monitor the progression of the individual and certain events that might be salient for a clinician to pick up and identify how to help that patient earlier than we would have otherwise been able to see.
Does this study have implications for costs associated with these kinds of behaviours in hospitals?
KB: Hematological malignancies are a global concern, right? No matter where you live in the world cancer is present. However, that doesn’t mean that we have equitable access to all the same resources. This was an important aspect that we looked at. Whether it was the limitations in next-generation sequencing, which very few countries have. Or multiparametric flow cytometry, which are expensive and complicated and require very sophisticated people to operate them. We were looking at more of the penny-per-cost test and that is what this is. It really is a low-cost preparation that doesn’t require a huge amount of skill. It does require a Raman instrument, but this is something that we deem could be affordable in most hospitals. But other than that, the training required to prepare the sample and input it is basic. Anybody could conceivably do that.
Once the system is up and running, it requires no additional training so there are no follow-on expectations, but blood handling being simple leads to the more complicated stuff that still needs a lot of work. So, it is not ready for prime time in the sense that we could just drop this in all hospitals, because we still need a lot more training and design engineering to go into that machine learning component. We need to build up our datasets and our standard process protocols to make it more ubiquitous, but I think that is a workable option and we are really excited by that because this is something that we think can be broadly taken up.
For a patient living with a condition such as multiple myeloma, what does this paper mean?
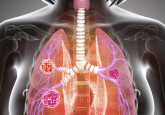
SG: We are still some way away from moving this into the clinic. But optimistically, this tool allows us with a simple blood test and a very small amount of blood to be able to monitor someone’s disease progression and pick up any changes not only specific to their disease, but maybe a treatment response or an adverse event, or some other biological phenomenon that is occurring because of their disease. So, for a patient, a quick blood draw means we can gather information about what is happening in their body, relevant to their disease and the physician can pick this up and decide we need to be more vigilant in how we are monitoring because we are seeing some changes, or the changes are enough that I think we need to start treating. Hopefully this will give the patient some peace of mind that their disease is being monitored without having to do any invasive test.
What are some of the next steps for incorporating Raman spectroscopy into clinical practice?
KB: I think one of the important things is to know that we have to build a better library and approach to the way we standardize this. It definitely requires a little bit more design engineering and certainly a lot more training. A machine learning algorithm is only as good as the training sets you are providing it and that is something that we really emphasize in this work, you don’t want to just have one training set, a reference set of healthy or even disease from an unrelated condition, you need quite a few different aspects.
Reproducibility is something the field really needs to focus on as generating another paper in another form of cancer with a slightly different modality is not the end goal here. The ultimate goal is to utilize these instruments and approaches. I think there are a few things, definitely the reference standards can be improved and the processes can be standardized. This is something we identified in the paper that conferences could be better suited to do and looking at how different instruments affect that. The ultimate goal is, we want this to work in Canada, South Africa, India, Japan, equally. That is really important to us.
We need to build our clinical indexes and evaluation criteria alongside that machine learning training too. We can’t just say somebody’s got a malignancy. We have to say what is the state of that malignancy. This is where Raman is so multifunctional because it can not only detect the nature of the cancer and the way the cancer is either being suppressed or inactive or resurgent. We can also find salient things related to the treatment itself. Whether that is an adverse event, potentially, or just in general, whether there are more aggressive signals.
We think that probably the best way to do this is to come alongside clinical trials that are actively recruiting because you have a good intake and follow through and a really nice clinical reference and data collection is ongoing there. And then, by working in tandem with that, we can use those clinical trial data to inform machine learning as well. That is really our next goal here to accelerate this and move this forward into a companion-like event.
SG: From a clinical perspective some of the things that we need to focus on are using validated clinical scales and running alongside clinical trials where we have known treatments and known responses, and we have a more homogenous group of patients that we can evaluate and train our machine learning algorithm on. I think we are very fortunate in New Brunswick that we have a researcher who is running a pan-Canadian myeloma study funded by the Terry Fox Research Institute (Vancouver, Canada) and hopefully we can access some of those samples because they are monitoring multiple myeloma patients in very controlled manner throughout the course of their disease from the diagnosis to the treatment, multiple treatment modalities and samples throughout the entire course of their disease.
This is very exciting and would allow us to take our paper, which is really a proven concept that we can use Raman to monitor disease, but to move it into the next step and prove that it is clinically relevant, and it might be an important component to include in clinical trials moving forward.
Any closing comments?
KB: In my career today, this is one of the most complex works I have ever engaged with, and I felt that this was truly an example of a diverse group of scientists, chemists, engineers, computerists, oncologists and biomolecular scientists really coming together in a way that none of us really knew what we were doing in its entirety. I think that is good, because all these highly specialized skills managed to work together and we generated this paper, and now this paper sort of serves as the foundation of our continuing work and Dr Grieve mentioned that already we are looking at one of these clinical trials with one of our partners.
We feel that drives innovation and solution creation. It is a small step, I agree, it is a proof-of-concept as Dr Grieve mentioned but it is high-risk and high-reward success that I think will continue to listen to our patient’s needs and understand what motivates them and what their needs are and then let our science be guided by that and that is really what started this. This was a high-risk, high-reward project and just bringing all of these people together as we go forward – the clinicians, the drug developers – looking at clinical chemistry, how does that system integrate within the hospital, and what engineers and biophysicists do we need to engage with? Stacey Grieve and myself as translationalists, this is a quintessential moment, where we are sort of looking at this paper why we actually did this. We got it all to come together, and we think we have given some good direction for the field as well.
The opinions expressed in this interview are those of the interviewee and do not necessarily reflect the views of Oncology Central or Future Science Group.