How can the LIO-1 study help to overcome challenges in gynecological cancer? An interview with Dr Erika Hamilton
Please can you introduce yourself, your research background and current research interests.
My name is Dr Erika Hamilton and I lead the Breast Cancer and Gynecologic Cancer Research Program for Sarah Cannon Research Institute at Tennessee Oncology in Nashville, Tennessee (TN, USA). I have been here for about 7.5 years and I am heavily involved in clinical trials, both from a Phase II and III standpoint as well as our drug development unit in Phase I.
What are the current challenges that need to be overcome in gynecological cancer treatment?
Gynecological cancers span several tumor types, including endometrial cancer (cancer of the uterus), ovarian cancer and cervical cancer. There is also this rare subset of sarcomas that come from gynecologic organs as well. I think one of the things that we have hoped would be the case is that we would see more benefit from immunotherapy in gynecologic cancers. There were certainly large ovarian trials, those reported have been negative thus far. We had hoped that because ovarian cancer has such a poor prognosis that it would be in the same camp of success as lung cancer, melanoma, kidney cancer etc., but I don’t think we have found the right combination yet.
Could you tell us about the LIO-1 study recently presented at ESMO 2020 and could you kind of give us an overview of the main findings of the trial?
LIO-1 was a Phase I dose escalation trial. It was a 4+3 design and 17 patients were treated with standard dosing of nivolumab, a checkpoint inhibitor, that’s given every 28 days. This was combined with increasing doses of lucitanib. Patients started at 6mg, this was tolerated, and then we moved to 8 mg and then ultimately went up to 10 mg.
Lucitanib is an oral tyrosine kinase inhibitor and inhibits a variety of things, including VEGFR-1, -2 and -3, PDGFR-α and -β, and FGFR-1, -2 and -3. In the 17 patients treated, we saw one complete response with a patient with anal cancer, and a partial response with a patient with cervical cancer. And then we had 10 additional patients that had stable disease and only three of the patients on this trial had progressive disease.
Adding lucitanib to nivolumab seemed to be an active combination, which was encouraging across multiple tumor types. We saw one dose-limiting toxicity and that was grade 3 proteinuria or protein in the urine. We also had a patient that had grade 3 hypertension at 6 mg, but we did not see any other dose-limiting toxicities of hypertension when we went to 8 mg or 10 mg. Common side effects were hypertension, fatigue, proteinuria and then also some mild GI effects, such as nausea or diarrhea.
How can this trial help to overcome some of the challenges previously mentioned, what does this mean for the field?
I think moving forward, the plan is to start patients at 6 mg of lucitanib in combination with nivolumab and then titrate up, meaning that if they get through the first cycle and they don’t have any significant adverse events that we would bump that patient up to 8 mg, and then again at the end of the second cycle, bump them up to 10 mg. This is due to a large inter–patient pharmacokinetic variability that we see. I am really calling this a kind of safety-based dose titration that’s going to move forward into the Phase II.
In the Phase II portion, we are looking to enroll up to 161 patients in four gynecologic cohorts. First endometrial cancer, second ovarian cancer, third is cervical cancer and then fourth is clear cell histology of either endometrial or ovarian origin. We are excited about this because of the activity that we observed in a small number of patients in the Phase I. We may be able to combine this tyrosine kinase inhibitor with immunotherapy to get more benefit for some of the gynecologic cancers that we haven’t seen a lot of benefit for with immunotherapy so far.
How do you see the field of gynecological cancers evolving over the next decade or how do you hope to see it evolve?
I think what we are seeing across a lot of cancer types, which I hope is going to be true for gynecologic cancer, is a move away from only having chemo in the recurrent setting. That is traditionally what we had and what we knew that works, but now we have many more targeted agents. We know that for microsatellite unstable tumors with a high tumor mutation burden, immunotherapy works. We have cancers in the gynecologic field that benefit from PARP inhibitors. We have drugs like Avastin, or bevacizumab, that inhibits VEGF.
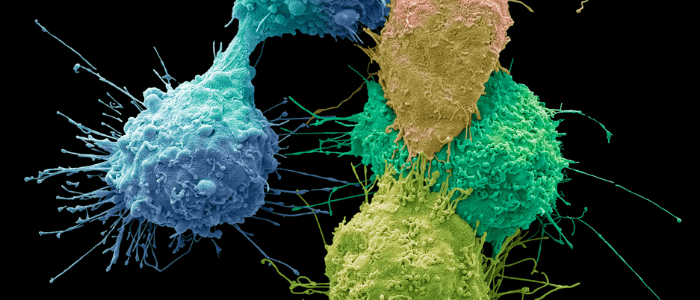
One class of drugs that I am excited about are antibody–drug conjugates and there are several that are being looked at for ovarian cancer. An antibody–drug conjugate is where we combine chemotherapy to an antibody through a linker so that it enables us to target a specific cancer cell and leave the rest of the body alone. I think this may be a more tolerable and specific way to target cancer cells.
The opinions expressed in this interview are those of the interviewee and do not necessarily reflect the views of Oncology Central or Future Science Group.