Coffee Chat highlights: the role of the microbiome in cancer diagnostics
The diagnostic implications of microbiome markers in tissue and liquid biopsies are endless, and Micronoma (CA, USA) is the first company developing a platform using these markers in blood to detect early-stage cancer. Our recent Coffee Chat explored the exciting and fairly new role of the microbiome in cancer diagnostics. Watch the Coffee Chat on-demand here whilst finding out key takeaways from our expert panel below.
What is the circulating microbiome and why is it so promising for early cancer detection?
- Recent research has shown that microbes live and are metabolically active within tumors.
- Each cancer type has a distinct community of microbes that live in that particular cancer type.
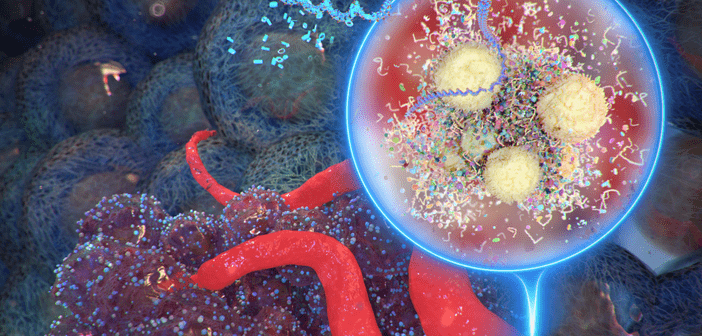
- Small quantities of the cancer microbiome sheds in blood, but it is a sufficient amount for detection.
- With a microbiome-driven liquid biopsy, we can detect both the presence of cancer and even the type of cancer.
Can you tell us more about your recent publication on profiling fungal communities in several cancer types?
- In our 2020 Nature paper we looked at more than 18,000 samples, more than 10,000 patients and 30 different cancer types. We took all that data and discarded all human DNA and RNA. In what was left, we searched for pieces of microbial DNA.
- Overall, 2−3% of sequence data was microbial, which translates to billions of microbial DNA and RNA reads.
- The research mostly focused on viruses and bacteria as they had the most complete databases at the time.
- In the recent 2022 Cell paper, we reprocessed the 2020 Nature paper samples focusing on the categorization of fungi in those samples.
- It is harder to identify fungi. Fungi is present in much lower abundances, there is approximately a 100:1 bacteria to fungus ratio.
- Utilized Weizmann Institute cohorts and substantiated the veracity of the findings.
- Also took a Johns Hopkins cohort and diagnosed cancer with better diagnostic performance than using human fragmentome.
- This Cell research provides the first atlas of fungi in multiple cancer types, thereby laying the groundwork for such mechanistic studies that could benefit future therapies and diagnostics.
How does a microbiome-driven biopsy compare to traditional ctDNA liquid biopsies?
- The traditional method of blood biopsy uses ctDNA, which is the detection of tumor derived genetic mutations that have been shed from the tumor and circulated in blood.
- Traditional ctDNA methods can detect the presence of cancer, but since ctDNA requires cell death/turnover, its quantity is a function of the tumor size. Early-stage tumors have low quantities of ctDNA. So, since these tests are dependent on size, late-stage cancers (stage III and IV) are more readily detected than stages I and II.
- Clonal hematopoiesis (CH) decreases the specificity of ctDNA. CH is when white blood cells get mutated during the normal aging process, and it creates a signal-to-noise issue on whether the signals are tumor derived or if they originate to white blood cells.
- On the other hand, cell-free microbial nucleic acids are completely independent of the cancer genome, and are not as impacted by cancer size. In addition, they allow us to sidestep the issue of clonal hematopoiesis.
- Microbiome based assays use shotgun metagenomic sequencing of all cell-free DNA in the sample, and we find a tremendous amount of microbial signal present (1−4%). This gives us a huge reservoir of microbial features that we can identify and with machine learning arrive at high complexity of microbial signatures.
- Driver mutations are harder to detect in early stages, since there are not that many markers (100s to low 1,000s of markers in the early stage of the disease). The diversity of the microbial features on the other hand leads to the benefit of the high sensitivity of a microbiome-driven test.
How does a microbiome-driven biopsy fit in the current standard of care in lung cancer diagnostics oncology?
- When we looked at entering this space we asked: “What would help physicians?” We are not screening a healthy individual but trying to diagnose a symptomatic patient. For example, given a pulmonary nodule, what is the status? Is it malignant or benign? A great opportunity for us to supplement the current standard of care, which is imaging and tissue-biopsy based.
- A large part of the current standard of care is to wait and see. If a nodule is detected under 3 cm, the current standard of care is to monitor and see if it is growing 3−6 months later. Given that tumors can divide and grow very quickly, this waiting period is a critical time where we can provide an answer.
- We hope to offer this assay for lung cancer next year.
In which ways can ctDNA- and microbiome-liquid biopsy tests be combined to enhance the detection of tumors?
- The microbiome is a human-genome-independent source of diagnostic information. So the opportunity is to synergize both the human component and pair that with microbial information. Because they are orthogonal, the benefit from both is going to provide great diagnostic synergy and the performance will be better together.
What is Micronoma’s current research pipeline focusing on early-cancer detection in microbiome-driven liquid biopsies?
- As far as lung cancer, in the U.S. there are 15 million people who are at risk for lung cancer and only 4−5% get screened. This contributes to lung cancer getting diagnosed so late. The goal is to use our technology to detect lung cancer earlier with a minimally -invasive blood test.
- On the research aspect, we will continue to develop these methodologies in other cancers. Pancreatic cancer, ovarian, liver, breast and colorectal cancer are part of our pipeline.
What are the other applications of microbiome driven cancer diagnostics?
- We decided to focus on early-cancer detection, but this is only the beginning.
- Residual Minimal Disease or relapse detection is in our pipeline as well.
- Finding the tissue of origin of metastasis is important, since you don’t treat the primary cancer the same way as the metastasized cancer that may carry their microbial load with them. This will help physicians with treatment selection.
- Can also find applications in new therapeutic pathways.
- Can identify failed drugs in trials that can be ‘rescued’ by doing restratification on the patients as high/low responders based on their microbiome. That would ultimately lead to new companion diagnostic applications.
What do you hope to see the field progress in the next five years?
Greg Sepich-Poore:
- We see a dynamic environment of fungi, bacteria and viruses within the cancer tumor at the same time as cancer cells and immune cells. So, what is happening to the cancer’s evolution? Looking at how cancers evolve over time and lead to treatment resistance or metastasis. These clonal evolution models do not currently include microbial information. How can we consider clonal evolution as a multi-species process? We have written a review paper on this topic, and it’s exciting to see the development of this.
Sandrine Miller-Montgomery:
- We are mining something that most scientists understand is much older than us and is a basic part of evolution. So, the comfort of using microbiome tests needs to come. We have the support of all this great science. Ultimately, we hope to get this platform into the hands of physicians.
- We all need to afford it or it cannot be used. A big focus is to help insurance/payers understand that there are huge cost savings with these diagnostics. It will cost less to the health care system and help patients lead productive lives.
Eddie Adams:
-
- On the lung cancer assay, I’m hoping for the development of a more multi-omic approach; next-level diagnostics that leverage the power of machine learning.
- Certain bacterial DNA is a potent immune stimulator – we see potent bacteria in healthy individuals. Understanding what mechanisms are at play that can lead to new therapeutic pathways?
In association with: