Beyond Wires: Overcoming the Challenges of Breast Tumor Localization
Executive Summary
Wire localization, the most common method for the surgical localization of nonpalpable breast tumors, is associated with a number of inherent procedural and outcome-related challenges. The most commonly reported include issues with scheduling, surgical planning and guidance, high re-excision rates and suboptimal patient experiences.
The SAVI SCOUT® surgical guidance system addresses many of the challenges associated with WL. US FDA-cleared in August 2014, the SAVI SCOUT system uses nonradioactive electromagnetic wave technology to detect a reflector that can be placed in the target tissue up to 7days prior to surgery.
SAVI SCOUT offers several benefits over current localization methods including nonradioactive technology, simplified scheduling, improved surgical planning and guidance and the potential for enhanced patient satisfaction. Outcomes from a recently completed investigator-initiated study demonstrate that the SAVI SCOUT system is a safe and effective tool for the localization of nonpalpable breast lesions and a viable alternative to wire localization.
The Need
Wire localization (WL) is the most common method for the surgical localization of nonpalpable breast tumors. Developed more than 20 years ago, WL has a number of inherent procedural and outcome-related challenges [1,2].
Market research conducted by the Breast Health Research Center* showed a significant level of dissatisfaction among breast surgeons with current tumor localization due to significant operational/procedural inefficiencies and a suboptimal patient experience. In fact, 93% of breast surgeons surveyed* want a better option for breast tumor localization. The most common challenges reported with current localization techniques include scheduling and workflow, surgical planning and guidance, high re-excision rates, and a suboptimal patient experience.
Scheduling and Workflow
Wire localization procedures take place on the same day as the surgical excision because part of the wire remains outside the patient’s breast. In many cases, the wire is placed in radiology, which impacts workflow, as this couples radiology and operating room (OR) schedules. Surgeons interviewed indicated that coordinating multiple procedures on the same day in different departments is difficult and leads to scheduling conflicts and inefficiencies:
- Long wait times for many patients – most localization procedures were reported to be in the morning only, while lumpectomy procedures continue through the afternoon. These time gaps are considered to be a contributing factor to unpleasant experience for the patient.
- Delays in the wire placement procedure or in the transport of the patient to the OR can put the OR behind schedule. Surgeons interviewed reported that delays happen in 0–95% of cases with the typical delay reported to be 30 minutes.
- Flexibility to begin surgeries earlier is an area of unmet need for most surgeons interviewed. Wire localization procedures begin at 7.30 or 8.00 am. As a result, lumpectomy procedures can’t start before 9.00 or 10.00 am.
Surgical Planning and Guidance
The ideal skin entry site for the radiographic placement of a wire may not be in close proximity to the lesion. As a result, the entry site of the wire may not correspond to the ideal location for the surgical incision, which is often made with cosmesis in mind.
Surgeons interviewed reported that a wire is an inadequate localizer because it limits the ability to optimally plan the incision site for the best cosmetic outcome:
“(With wire localization) you have to be creative about placing your incision. I was trained to come straight down on the wire, but that can mean you go through a lot of normal breast tissue to get to where you’re going.” – Breast surgeon, The American Society of Breast Surgeons (ASBrS) Meeting, 2014.
Re-Excision Rates
Surgeons interviewed report re-excision rates of 5–60%, which corresponds to reports of high variability in the literature ranging from 0–60% [3,4], depending on surgeon skill, geography, patient age and tolerance for margin.
Reasons cited by surgeons interviewed include:
- Migration of wires during patient transport
- Difficulty locating the end of the wire
- Wires transected during the surgical dissection
“It’s like trying to find a needle in a haystack.” – Breast surgeon, American College of Surgeons (ACS) Meeting, 2011.
Patient Experience
Surgeons also reported long wait times and significant patient discomfort associated with wires:
- Wire localization procedures are typically scheduled in the morning, while lumpectomy procedures can continue through the afternoon. This can mean an early morning localization procedure for some women, with several hours of waiting with ‘wires hanging out of their breasts’.
- Scheduling the two procedures on the same day requires very careful planning to provide the patient with proper care. This can also lead to longer wait times from diagnosis to surgical excision.
The Solution: SAVI SCOUT® Surgical Guidance System
The SAVI SCOUT® Surgical Guidance System is a technological advance in tumor localization. FDA-cleared in August 2014, the SAVI SCOUT system uses nonradioactive electromagnetic wave technology to detect a reflector that is placed in the target tissue up to 7 days prior to surgery. The system uses real-time audible and visual indicators to give surgeons a precise way to locate the micro-reflector and tissue targeted for removal during lumpectomy and excisional biopsy procedures. The components of the system include:
- Electromagnetic wave reflective device (reflector) – implantable device that can be percutaneously placed into the area targeted for removal up to seven days prior to the excisional procedure.
- Handpiece – emits nonradioactive electromagnetic waves. Used to detect and confirm the location of the reflector from the surface of the patient’s breast.
- Console – provides audible and visual feedback that increases in cadence with the proximity of the reflector to the handpiece.
SAVI SCOUT offers several benefits over current localization methods including nonradioactive technology, simplified scheduling, optimal surgical planning and guidance, and enhanced patient satisfaction.
Nonradioactive Technology
Radioactive seed localization (RSL) has been described as an alternative approach to address the number of clear disadvantages associated with WL [1,2]. Yet, despite its proven advantages, the adoption of RSL has been impacted by considerable regulatory requirements for the safe handling of radioactive materials. SAVI SCOUT has been developed to advance the progress made with RSL and eliminate the considerable administrative and handling issues associated with radioactive components.
Easier Scheduling and Increased Workflow Efficiency
The reflector can be placed at the tumor location up to 7 days prior to surgery. This flexibility uncouples OR and radiology schedules to result in a simplified workflow that eliminates challenges caused by multiple same-day procedures in different departments. The ability to place the reflector on a day prior to surgery allows radiology to schedule patients as needed throughout the day and allows operating rooms to schedule lumpectomy or excisional biopsy procedures early in the morning. As a result, this flexibility may improve OR efficiencies and allow for significant cost savings and potential increased revenue opportunities.
Optimal Surgical Planning and Guidance
The electromagnetic system allows the location of the reflector to be confirmed before an incision is made. The location of the handpiece on the patient’s skin that provides the highest-cadence audible signal is the location of closest proximity to the reflector. This precision provides confidence and allows the surgeon to plan an optimal incision location.
Once the skin incision is made and dissection begins, the handpiece and console guide the localization and removal of the reflector along with the surrounding breast tissue. This real-time feedback removes the guesswork involved in locating the target and allows for continuous adjustment of the direction of dissection. This has the potential to result in better cosmesis, added surgical confidence, and lower re-excision rates. As a final verification step, the handpiece can be applied to the excised specimen to confirm removal of the reflector.
Better Patient Experience
This surgical guidance system has the potential to improve the patient experience in several ways. Because the reflector is implanted within the breast tissue, anxiety regarding device movement is reduced. In addition, placing the reflector on a day before surgery creates a shorter surgical day for the patient, minimizes anxiety caused by two procedures on the same day, and eliminates transportation between radiology and surgery.
Physician Reaction to New Concept for Breast Tumor Localization*
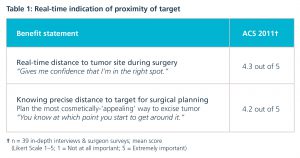
Surgeons and radiologists were surveyed* on the concept of an electromagnetic wave device for breast tumor localization that would provide real-time guidance during removal of non-palpable breast lesions. The following tables summarize physician ratings and reactions to the potential benefits of the concept.
Table 1: Real-Time Indication of Proximity of Target
Table 2: Potential to Reduce Re-Excisions
Clinical Perspectives
A pilot study (n = 50) was conducted to determine the technical feasibility, safety and efficacy of SAVI SCOUT in localizing and directing the removal of nonpalpable breast lesions during lumpectomy and excisional biopsy procedures. The data from the study show this surgical guidance system to be a safe and effective tool for tumor localization [5]. A second, extended trial will validate these findings with planned enrollment of a total of 200 patients at up to ten sites.
Charles Cox and Pat Whitworth, the first two surgeons to utilize SAVI SCOUT, share their perspectives based on their early clinical experience with the technology.
Breast surgeon, Charles Cox, MD, The University of South Florida Breast Health Program in Tampa (FL, USA)
Charles Cox is the Lead Investigator of the SAVI SCOUT Pilot Study. He is also one of the innovators of RSL.
“This is very similar to Radioactive Seed Localization. But there’s no regulatory deterrent due to radiation. That’s huge.”
In what way did the challenges of breast tumor localization motivate you to develop RSL?
We developed RSL to resolve the challenges associated with WL. Compared to WL, RSL saves significant OR time and costs. If the wire localization is not done at exactly the right time, it can put the OR schedule way behind. It’s a huge expense to have OR staff waiting for patients – six jobs are impacted by OR delays – surgeon, scrub tech, circulating nurse, anesthesiologist, anesthesiology assistant, surgical assistant. A radioactive seed can be put in up to 5–7 days in advance, eliminating the need to schedule radiology placement and OR time on the same day, thereby eliminating OR delays caused by wire placements.
Another issue we experienced with wires is that following wire placement, recompression of the breast can result in the wire being pushed deeper into the breast tissue, altering the localization and requiring excision of excessive tissue to remove the wire. When embedded in the breast, the radioactive seeds cannot be displaced by breast compression. The radioactive seed is embedded in the breast, so it doesn’t get dislodged.
Compared to WL, we have found that RSL does a better job of targeting the lesion for removal. It’s a big problem for a patient when you tell her that you have to go back to get a better margin; the patient thinks, ‘Well, you’re not a very good surgeon.’ With RSL, we remove less tissue with a 30% better margin excision.
What has been your experience with the SAVI SCOUT Surgical Guidance System?
The SAVI SCOUT system gives you options for planning your surgical approach. Like RSL, SAVI SCOUT does not limit the placement approach – the radiologist can place the reflector from any direction. With WL, the wire often goes tangentially toward the end of the lesion through the breast. Knowing the general location of the end of the wire and trying to make your incision directly over this location does not always pan out and you end up removing a lot more tissue.
Like RSL, the big advantages with this are timing of the procedure, speed of detection and being able to direct the incision to the precise target site. The reflector can be quickly detected from the surface of the patient’s skin, which allows you to make a direct incision. A direct approach is more cosmetic, less deforming, and results in less tissue removal.
Describe your surgical technique with this new guidance system.
SAVI SCOUT uses electromagnetic waves that are designed specifically to work in breast tissue. The handpiece, when placed on the breast surface, transmits the signal to the reflector through the tissue. Scanning the surface of the breast with the handpiece allows the electromagnetic waves to detect the reflector. There is a slight delay between moving the handpiece and receiving the audible feedback, so you need to move the handpiece slowly and deliberately to detect the reflector – this is the biggest part of the learning curve. It takes less than five cases to refine the technique; after four or five cases it becomes intuitive.
The system is directional as the handpiece picks up the reflector when it is pointed in the direction of the reflector. Tilting the handpiece from side to side, away from the reflector, provides a lower signal. Aligning the handpiece with the reflector maximizes detection and allows a direct dissection.
What is your perception of the patient experience with this surgical guidance system?
Like RSL, this is easier and more comfortable for the patient. Patients don’t complain because there is nothing sticking out of the breast. Wires cause a lot of anxiety for patients – they worry about it getting dislodged, pulled out or pushed in.
Breast surgeon, Pat Whitworth, MD, Nashville Breast Center (TN, USA)
Pat Whitworth is a Principal Investigator of the SAVI SCOUT Pilot Study. Currently, he primarily uses intraoperative ultrasound (IOUS) for tumor localization.
“This is an obvious improvement in targeting. We have precedent for believing that better, more confident, more certain targeting results in less tissue taken out with equivalent margin control.”
In what ways does using IOUS help overcome the challenges that you experienced with tumor localization?
For many years, we have advocated using IOUS to guide our dissection and surgery; with IOUS you can get much better guidance than just guessing where the wire is and trying to dissect down to it. Studies show that the better guidance the surgeon has, the less volume of tissue you take out.
With wires, you don’t really get any tactile feedback about where the tumor is in the breast. Even with IOUS, it’s helpful to have some additional guidance; for certain lesions, I use a long, 18-gauge needle placed under ultrasound guidance to get some tactile feedback.
What has your experience been like with the SAVI SCOUT® Surgical Guidance System?
I use IOUS to place the marker in the OR prior to the lumpectomy procedure. Intraoperative ultrasound guidance is cumbersome compared with using SAVI SCOUT – with IOUS, you have to remove your retractor, turn the lights down, stop to get a look, put the ultrasound probe down, put your retractor back in place. With SAVI SCOUT, everything is retracted and held in place. I can be ready to make the next cut through the tissue, grab the handpiece and make the cut more precisely in reference to the target.
I find this to be more precise in reference to the target with the immediate real-time feedback as to where your target is as you are cutting through the tissue. This adds to my confidence tremendously because IOUS can be a little hard to interpret as you are going through a complex specimen and the lesion is not that easy to see to begin with.
With the reflector in position, you get feedback through the entire case easily. I’m far less concerned about getting to target tissue and not having to take too much extra normal tissue just to be sure of capturing the target because I know I can get right down to it, even if it’s in the back of a very large breast.
And like most cases using IOUS, we don’t need to coordinate scheduling of the two procedures, so it also puts surgeons in a position to do an 8.00 am procedure vs starting at 9.00 or 10.00 am.
Describe your surgical technique with this new guidance system.
One of the main things that I found is that you need to get used to the speed at which moving the handpiece off of the target registers in the audio feedback. If I move off the target, the audio feedback goes to a lower frequency; that change in frequency takes a second or two. You need a slow, deliberate motion to give the system time to react.
Most surgeons are already used to that kind of feedback with sentinel node biopsies. SAVI SCOUT works similarly to the handheld lymphoscintigraphy probe: if you’re right on the target, you get a high-pitched signal; if you move off the target, the high-pitched signal stays there for a second before it trails off.
What is your perception of the patient experience with this surgical guidance system?
Wires are another insult to the patient – a wire sticking out, taped on the chest. With this new guidance system, you don’t get out of having to have a procedure, but at least you don’t have a wire sticking out of the breast. The SAVI SCOUT reflector can be put in any time up to 7 days before surgery at the patient’s convenience; it doesn’t have to be on that day of the procedure; they don’t have to walk around or roll around with a wire sticking out of the breast; it’s convenient and more comfortable for patients.
Conclusion
The options for the surgical excision of nonpalpable breast lesions have expanded with the FDA’s clearance of the SAVI SCOUT surgical guidance system. The system uses nonradioactive electromagnetic wave technology to provide real-time guidance during lumpectomies and excisional biopsies. SAVI SCOUT offers several benefits over current localization methods including nonradioactive technology, simplified scheduling, optimal surgical planning and guidance, and enhanced patient satisfaction.
Data from the Pilot Study [5] show SAVI SCOUT to be a safe and effective tool for the localization of nonpalpable breast lesions and a viable alternative to WL. The study resulted in 100% surgical success and yielded a re-excision rate in line with those reported for RSL and IOUS.
A larger prospective, single-arm, multisite, clinical evaluation of SAVI SCOUT for the location of nonpalpable breast lesions during excision is currently underway.
Case Study
Case: 60-year-old female scheduled for lumpectomy of a right breast lesion
Diagnosis: Invasive ductal carcinoma, T1, NO, stage 1, <3 cm, right breast
Localization: Three days before the scheduled surgical excision, a radiologist placed the SAVI SCOUT reflector with mammographic guidance. In the medial-lateral image, the biopsy site marker can be seen at coordinates G-5. With the breast under compression, the SAVI SCOUT delivery system, preloaded with a reflector, was advanced into the skin at the aforementioned coordinates. The breast was then released from compression and repositioned in compression in the cranial-caudal direction. The needle position was adjusted to place the needle tip 1 cm past the biopsy marker to ensure accurate delivery of the reflector. Upon delivery, the reflector was located 6 mm from the biopsy marker. Following placement, the surgeon confirmed the detectability of the reflector with the handpiece and console.
Surgical Planning: In the OR, location of the reflector was confirmed with the handpiece and console. Once confirmed, the surgical incision was planned.
Surgical Guidance: The time from skin incision to specimen removal was 11 minutes.
Removal Confirmation: The hand piece was placed on the excised specimen to confirm removal. Specimen radiograph further confirmed removal.
Results: Pathologic results showed clear margins. Compared to WL, surgeon rated the ease of localization better than wires.
*Primary market research on new surgical guidance system
From 2011–2014, 78 interviews or surveys were conducted to assess feasibility and reaction to concept of Implantable Electromagnetic Wave Reflective Device for breast tumor localization in breast conserving therapy. Sixty of these interviews were conducted with breast surgeons, defined as > 25% of their surgical practice devoted to breast. Interviews were conducted at the ACS meeting in 2011, the ASBrS Meeting in 2014, and in individual surgeon’s institutions from 2011–2014. Research was conducted by the Breast Cancer Research Center, a division of Motivation Mechanics LLC, paid for by Cianna Medical.
References
- Hughes JH, Mason MC, Gray RJ et al. A Multi-Site Validation Trial of Radioactive Seed Localization as an Alternative to Wire Localization. The Breast Journal 2, 153–157 (2008).
- Jakub JW, Gray RJ, Degnim AC et al. Current Status of Radioactive Seed for Localization of Non Palpable Breast Lesions. The American Journal of Surgery 199, 522–528 (2010).
- Esbona K, Li Z, Wilke LG. Intraoperative imprint cytology and frozen section pathology for margin assessment in breast conservation surgery: a systematic review. Ann Surg Oncol. 19(10), 3236–3245 (2012).
- Wilke LG, Czechura T, Wang C, et al. Repeat surgery after breast conservation for the treatment of stage 0 to II breast carcinoma: a report from the National Cancer Data Base, 2004-2010. JAMA Surg 149(12),1296–1305 (2014).
- Cox CE, Whitworth P, Cox JM, et al. (2015, March) Pilot Study of a New Non-Radioactive Surgical Guidance Technology to Localize Non-Palpable Breast Lesions. Poster presented at the National Consortium of Breast Centers 25th Annual Interdisciplinary Breast Center Conference, Las Vegas, NV.
About the Authors
Charles Cox, MD, USF Breast Health Program
Charles Cox is Director of the Comprehensive Breast Cancer Program at USF in Tampa, FL. He and his colleagues spearheaded the research and training in the technique for Lymphatic Mapping and Sentinel Lymph Node Biopsy in breast cancer patients. Along with his pathology colleagues, they developed the Intra-Operative Touch Preparation Cytology for the evaluation of surgical margins. With these techniques, they have experienced high success rates in breast conservation and lymph node sparing. Dr Cox is also one of the innovators of RSL for tumor localization in breast conserving surgery.
Pat Whitworth, MD, Nashville Breast Center
Pat Whitworth is Breast Surgical Oncologist and Director of the Nashville Breast Center in Tennessee. He is a pioneer in new methods of breast tumor localization that both improve the surgical outcome and the patient experience. Among his clinical interests are cancer genetics, targeted treatments, minimally invasive surgery, and breast oncoplasty. Some of his recent work and publications include advancing and expanding the use of genetic testing by breast surgeons to aid in decision-making and optimal patient treatments.
Kate Maguire, President, Motivation Mechanics
Kate Maguire leads a team of market researchers on a myriad of investigations regarding new product viability, product positioning, context for decision-making and overcoming barriers to trial and usage. Her research and strategy have helped open doors to new categories and care paradigms, including disposable contact lenses, laser vision correction/LASIK, cervical cancer screening/STD screening, brachytherapy, in-office treatment for heavy menstrual bleeding, and numerous products related to prenatal testing and patient management.