A peek behind the paper – Hilary Marusak on pediatric cancer and fear-related neural circuitry
Take a look behind the scenes of a recent International Journal of Hematologic Oncology review, entitled ‘Pediatric cancer, posttraumatic stress, and fear-related neural circuitry’, as we ask lead author Hilary Marusak (Wayne State University, MI, USA) what can be done to reduce the risk of pediatric cancer patients developing PTSD, the greatest challenges in this area of psycho-oncology and what the future might hold for this field.
Could you introduce yourself and explain what began your interest in researching the neurological effects of pediatric cancer?
I am a developmental neuroscientist at Wayne State University and my research focuses on the effects of stress and trauma on brain development in kids. It is not surprising that pediatric cancer is a stressful and potentially traumatic experience for children and their families, and many will consequently experience posttraumatic stress symptoms (PTSS) or posttraumatic stress disorder (PTSD). Yet, as a developmental neuroscientist, I was surprised to learn that very little research has considered the impact of the stressful or traumatic aspects of pediatric cancer on brain development. My prior research has shown that exposure to other types of stressful or traumatic experiences in early life, such as witnessing violence or experiencing abuse, has profound effects on brain development. In addition, these changes in brain development may help to explain why exposure to stress and trauma in early life dramatically increases risk of anxiety, depression, and PTSS/PTSD. With more children surviving pediatric cancer today than ever before, it is crucial to understand how this experience affects the developing brain and how we can prevent PTSS/PTSD and other negative outcomes throughout the lifespan.
Could you give a short overview of what you discuss in your review?
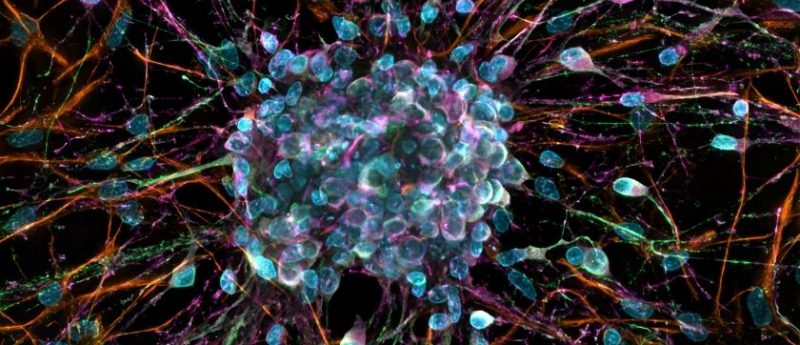
The mini-review looks at PTSS and PTSD in pediatric cancer, and considers the impact of this experience on brain development. In particular, we examine fear circuitry in the brain, and how changes in this core circuitry may predispose some children or their family members to PTSS/PTSD.
What can be done to reduce the risk of a pediatric cancer patient developing PTSD?
To reduce the risk of a pediatric cancer patient or family member developing PTSD/PTSS, there should be an emphasis on preventive psychosocial support for patients and families – throughout the cancer trajectory. That means that there should be support for families at the time of diagnosis, through treatment, and importantly, throughout survivorship. So often, we hear from families that support drops off after treatment concludes, or when children hit their 18th birthday and are no longer are seen for follow-up care in a pediatric clinic.
We know that PTSD/PTSS can affect children and their families decades after the conclusion of treatment. Several outstanding support professionals and organizations exist that can help children and their families cope with the disease, diagnosis, treatments, and side effects, and can thus help to reduce the risk of PTSD/PTSS. This support can include social workers, psychologists, child life specialists, and non-profit organizations such as Kids Kicking Cancer. However, these support staff can be costly and there are often not enough to provide adequate support to all families. Thus, we need to support these organizations and professions, and fund research that aims to develop and test the most effective programs or interventions for preventing PTSD/PTSS.
What do you think the greatest challenges are in this area of psycho-oncology and how could these be overcome?
One challenge for psycho-oncology research is identifying the factors that can increase risk of, or protect against, the development of PTSD/PTSS or other adverse outcomes. This is a ‘chicken or the egg’ problem, and affects research on stress and trauma more generally because we often don’t have a chance to study children and families before the potential trauma happens (i.e., before diagnosis). So we don’t know if children or families had some risk factor that existed prior to their diagnosis, that increased their risk of subsequently developing PTSD/PTSS.
In addition, because we work with human beings who are very complex, it is hard to identify the factors that can increase risk or protect against PTSD/PTSS. Another complication is the influence of treatment-related factors. We know from our prior research that exposure to stress and trauma in early life has dramatic effects on brain development. However, the medical treatments for pediatric cancer – chemotherapy and radiation therapy – have also been shown to have profound effects on the brain. Therefore, it is very hard for us to tell which of these factors – the stress or the cancer treatments – are causing the changes we see in the brain. It is very challenging to disentangle these effects, since these factors do not often occur alone. That is, it is unlikely that a child receives treatment for cancer but does not experience any stress or vice versa.
What are your predictions for future of this field?
I hope and predict that the field of psycho-oncology will continue to benefit from the ever-growing body of research on brain development and the effects of stress and trauma on the brain and mental health outcomes. This knowledge can be used to better understand PTSS/PTSD and other mental health consequences, and to design and test interventions that can prevent their development.