Unlocking the promise of clinical immunotherapy – a conversation with James Gulley

Oncology Central recently spoke with James Gulley, Director of Medical Oncology Service at the National Cancer Institute (NCI), about his work developing cancer immunotherapies, his insights into the impact of this modality in prostate cancer and his hopes for the future of the field. Discover more below, including details of an early stage trial of a next generation, bi-functional immunotherapy agent with two distinct mechanisms of action.
Could you briefly summarize your career to date & your role at the Medical Oncology Service for Cancer Research?
- I have been at the NCI since 1998, running immunotherapy clinical trials for patients with cancer. I have focused on therapeutic vaccines, immune checkpoint inhibitors, immunocytokines and combination approaches. I also run the Medical Oncology Service at the NCIs Center for Cancer Research and am the Chief of the Genitourinary Malignancies Branch.
You are the lead investigator for the Phase I clinical trial for a novel immunotherapy termed M7824. The aim of this trial is to investigate the safety and tolerability of M7824. Can you provide us with a brief overview of your findings?
- This first-in-human study has demonstrated that this agent – M7824 – can be safely administered at doses of up to 20 mg / kg every 2 weeks in patients with advanced cancer.
It is associated with two distinct mechanisms of action – binding to PD-L1 (thus blocking negative signals to T cells including one targeting the tumor) and neutralizing TGF-β. It does the latter by binding and sequestering activated TGF-β so it is not available to send negative signals to immune cells and tumor cells.
Finally, the agent has been associated with decreases in tumor size in some patients with several patients having prolonged stable disease, a patient having prolonged partial response and another having a sustained complete response.
What do these results mean for patients?
- This means that for the first time, patients may have access to an agent that targets two important mechanisms of immune suppression present within the tumor with a single agent.
We have long known that TGF-β is an important cytokine that shuts down a therapeutic antitumor immune response. However, to date, no TGF-β-targeted therapy has been US FDA approved. This unique agent combines the known activity of blocking the PD-1/PD-L1 interaction with decreasing activated TGF-β and thus for the first time we have a bi-functional agent targeting cell-intrinsic and cell-extrinsic mechanisms of immune suppression. These initial promising results with this agent are providing the impetus for further clinical testing.
What do you see as the next steps in the development for M7824?
- Two patients with good evidence of benefit have HPV-associated cervical cancer. Thus there is a possibility of improved responsiveness in patients with viral-associated cancers. In addition, one patient with pancreatic cancer had a sustained response. So there may be cancer types outside of the tumors thought to be generally responsive to PD-1/PD-L1 inhibition that respond to M7824 as a single agent.
However, my bias is that there may be even greater activity when this agent is combined with other agents (e.g., therapeutic vaccine, radiation or chemotherapy). I see that as an area that I will be enthusiastically exploring.
In your opinion, is there a particular patient profile that would benefit most from M7824?
- It is too early to rule out any patient population, but thus far HPV-positive tumors appear promising. It is not clear if tumors associated with TGF-β activation will be more responsive; however, there are a broad range of tumors where TGF-β signalling is associated with worse outcomes.
Dr Gulley also played a played a key role in the development of therapeutic vaccines for prostate cancer – we took this opportunity to explore his work in this area a little further.
How has the management of prostate cancer changed over the last decade?
- The treatments for prostate cancer have changed dramatically over the last 7 years. We went from one drug shown to impact overall survival in metastatic castration-resistant prostate cancer to six drugs. This started with the approval of sipuleucel-T (a therapeutic vaccine) but went on to include other chemotherapy, androgen receptor-targeted therapy and bone-targeted therapy.
You played a central role in the clinical development of prostate cancer vaccines. Can you tell us about how this field has developed over the past decade?
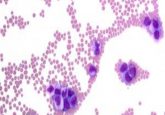
- Prostate cancer is a T-cell poor tumor, meaning that few cancers generate underlying immune responses. That is a likely reason for why the immune checkpoint inhibitors do not lead to activity by themselves in patients with prostate cancer. Therapeutic vaccines against prostate cancer could lead to a robust immune response against tumor targets. It is possible that the T cells could impact clinical outcomes (like overall survival). It is also possible that this could be enhanced with immune checkpoint inhibition.
What success and obstacles have you encountered in the field of prostate cancer vaccines?
- The major successes seen with therapeutic vaccines for prostate cancer include improvements in overall survival with minimal side effects of the therapy. This has been seen with sipuleucel-T and preliminary data suggests improvements in overall survival with Prostvac also.
The Phase III study for Prostvac completed accrual in January 2015 and overall survival data are expected as early as later this year. However, these data come with important caveats. Patients and their providers need to understand not to expect dramatic sustained decreases in PSA or improvements in symptoms with these therapeutic vaccines alone. On the other hand, there is an apparent slowing down in the growth rate of tumors, driven by the continued immune pressure, which leads to improved overall survival.
You have previously spoken about combining vaccines with immune checkpoint inhibitors in order to intensify the immune response. Can you tell us more about this method and whether it has proved successful?
- There is much promise in combining vaccines with immune checkpoints. In order for an optimal antitumor immune response, one must both be able to generate tumor-targeted immune cells (e.g., via vaccination) and allow those cells to work optimally within the tumor (e.g., immune checkpoint inhibition).
We know from studies of sipuleucel-T that this vaccine is associated with an increase in T cells at the tumor/normal interface. However, activated T cells will lead to upregulation of PD-L1 on tissue/tumor cells thus limiting the killing activity of the T cells. Adding agents that can block these checkpoints from interacting with the T cells will allow those T cells to carry out their activity unimpeded. Initial studies that will further identify the clinical utility of this approach are ongoing.
Can you tell us about some of the emerging concepts in prostate cancer immunotherapy?
- My favorite direction remains combination of vaccines with immune checkpoint inhibitors. However, there are other unique combinations that we are starting to see early signals of activity. Promising clinical data are emerging about enzalutamide and pembrolizumab in patients that have failed enzalutamide alone.
Another very early story involves combining a PARP inhibitor with PD-L1 inhibition. I think we will continue to see novel combination therapies being tried with rapid expansion of any clinical signals seen. I would also add that a PSMA CAR-T cell approach will begin enrolling prostate cancer patients in the first half of this year. This could lead to inflamed tumors and may open the way to combination therapy approaches.
Where do you hope to see the field in 10 years’ time?
- I hope that in 10 years we will have multiple new agents that can not only decrease tumor and improve overall survival, but can lead to cure. Obtaining the long-term durable responses will likely involve immune-based approaches with strategic use of agents that can both ignite an immune response and ones that can overcome the many immune regulatory influences within the tumor microenvironment. TGF-β is an important immune-suppressing cytokine that is present in a large number of cancers.
Do you have any closing comments for our readers?
- My patients love the idea that we are giving them agents that can help their body’s immune system fight their cancer. And as promising as this idea is now, our current approaches only help a minority of patients.
Despite only seeing responses in a minority of patients, because of the deep and durable responses seen, companies and academics are devoting large amounts of resources to this field. However, I believe we have only begun to unlock the promise of what clinical immunotherapy has in store. By understanding the impact of these therapies on the tumor, we can adjust therapies to maximize their impact. The current generations largely of single agent immunotherapy will likely be replaced by more effective double and triple combinations.
Biography
Dr. James Gulley, MD, PhD, is Chief, Genitourinary Malignancies Branch; Head of Immunotherapy Section; Director, Medical Oncology Service, National Cancer Institute (NCI). Dr. James Gulley is an internationally recognized expert in cancer immunotherapy with a strong interest in prostate cancer. Since 1998 he has authored and run a variety of clinical trials at the NCI. These innovative investigator initiated studies involve the use of cancer vaccines and other immunostimulatory agents, and the combination of immunotherapy with other treatment strategies. In particular, he has played a central role in the clinical development of a prostate cancer vaccine (Prostvac), created in the NCI, and serves as the principal investigator on an international Phase III randomized clinical trial of this vaccine. He is also the coordinating principal investigator of an international trial of an anti-PDL1 antibody (avelumab) and another international study of anti-PDL1 / TGF-beta Trap (M7824). Areas of Expertise are immunotherapy, therapeutic cancer vaccines, immune checkpoint inhibitors, prostate cancer, clinical trials, combining immunotherapy with other therapies.
The opinions expressed in this interview are those of the interviewee and do not necessarily reflect the views of Oncology Central or Future Science Group.