Optimizing post-procedural imaging – interview with Tobias Jakobs
As part of our spotlight on Interventional Oncology, Oncology Central spoke with Tobias Jakobs from the Hospital In the Order of St. John of God (Munich) about his thoughts on DC Bead LUMI™ including how it may aid post-procedural imaging.
With the launch of DC Bead LUMI™, do you think your approach to treatment will change?
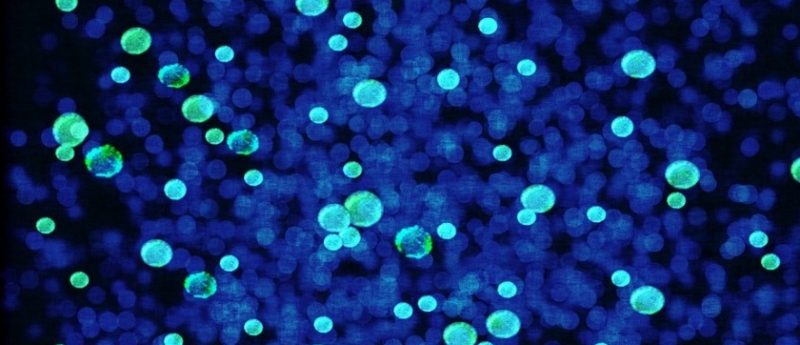
I think my treatment approach will change in the sense that I can basically prove where I treated my patients. For me, this will probably mean that I will double check during the treatment whether I targeted the whole tumor or if there are any parts of the tumor missing. I think it will increase my confidence that I will be able to cover the tumor in its entirety. We can now really demonstrate that we are able to super-selectively target the tumor. We are not utilizing any surrogate markers such as lower perfusion. We also do not need to wait for imaging follow up studies. We can instantaneously prove that we have covered the whole tumor.
Presumably knowing bead location provides you with more control?
I am looking forward to using this device as I am curious to see during follow up imaging which parts of the tumor responded well and which parts of the tumor did not respond very well to treatment. This may provide me with an idea of whether I undertreated a tumor. I have some markers which tell me that I require a certain density of LUMI within the tumor to achieve complete response etc. This is something I would like to see, to have more markers which help guide me during the patient’s treatment.
What about post procedure imaging with DC Bead LUMI™?
I think this is a very important point because currently, when clinicians are treating patients they are in a rush, as the contrast staining within the drug eluting beads usually washes out within a certain period of time. Especially in multi-focal disease, clinicians might miss this contrast staining in previously treated tumors. This means we may not be sure when we want to perform imaging. But now, with post-procedure imaging with LUMI, clinicians can conduct post-procedural imaging 10 minutes after embolising the tumor, an hour after or even the next day. This gives us more room for treating our patients.
Do the post procedure images support your discussions with the tumour board?
Proving my superselective treatment to my partners in the tumor board is exactly what I want to use LUMI for. I can now demonstrate the effect through images. For example on conebeam CT images I can demonstrate that I have treated the tumor completely and that no parts of the tumor are missing. It enables us to see LUMI in the tumor and surrounding tumor-feeding arteries. This will enhance my position in the tumor board as they realise that the interventional radiologist is really covering the whole tumor.
How might the visible evidence help in your discussions with your patients?
Well, what I would first discuss with my patients is that I am using a device which I can actually see. This would make perfect sense to the patient because they want me to use a device which I can see in order to perform precise treatment. I believe that the patient would be very happy if I offer this treatment option. In addition, if I can show the patient really clear images, post procedural imaging studies within which we can identify the tumors, through this I could demonstrate for example that I did not treat the non-tumor bearing liver tissue, I specifically treated the tumor – I think the patient would really appreciate this.
This will refine my treatment and at least it will probably alter the way of imaging during treatment. First of all I may want to use images to visualize where LUMI is being lodged in the tumor. Secondly I would probably adopt a different protocol in utilizing conebean CT during the treatment. I am looking forward to using DC Bead LUMI™ in my daily practice.
Profile:
Tobias Jako bs began his studies of human medicine at the Georg-August-University (Göttingen, Germany). After studying at the University of Vienna (Austria) and the University of California in San Francisco (CA, USA), Jakobs presented at Ludwig Maximilians University (Munich, Germany) in 2001 and was promoted 3 years later. In 2008 was Jakobs as a scientific assistant at the Institute of Clinical Radiology of the Clinic of the University of Munich (Germany). From 2008 to 2010 he was a senior physician and area manager of angiography and interventional patients radiology, also at the Institute of Clinical Radiology at the University of Munich. During this time, he received his medical doctor’s certificate in radiology. In 2011 Jakobs moved to the Hospital In the Order of St. John of God (Munich) Diagnostic and Interventional Radiology. He is also a member of the Radiological Society Community practice Dres. Wachter, Egge, Rieger and Jakobs. In addition to his work as a doctor, Jakobs is an intensive author. Many of his more than 170 publications have been published in renowned medical journals. He is also engaged in numerous national and international specialist companies, among others; the German Radiological Society (DRG), the German Society of Interventionists Radiology (DeGIR) and the Radiological Society of North America (RSNA). Beyond that he worked as a consultant for various trade journals.
bs began his studies of human medicine at the Georg-August-University (Göttingen, Germany). After studying at the University of Vienna (Austria) and the University of California in San Francisco (CA, USA), Jakobs presented at Ludwig Maximilians University (Munich, Germany) in 2001 and was promoted 3 years later. In 2008 was Jakobs as a scientific assistant at the Institute of Clinical Radiology of the Clinic of the University of Munich (Germany). From 2008 to 2010 he was a senior physician and area manager of angiography and interventional patients radiology, also at the Institute of Clinical Radiology at the University of Munich. During this time, he received his medical doctor’s certificate in radiology. In 2011 Jakobs moved to the Hospital In the Order of St. John of God (Munich) Diagnostic and Interventional Radiology. He is also a member of the Radiological Society Community practice Dres. Wachter, Egge, Rieger and Jakobs. In addition to his work as a doctor, Jakobs is an intensive author. Many of his more than 170 publications have been published in renowned medical journals. He is also engaged in numerous national and international specialist companies, among others; the German Radiological Society (DRG), the German Society of Interventionists Radiology (DeGIR) and the Radiological Society of North America (RSNA). Beyond that he worked as a consultant for various trade journals.
Disclosures:
- Speaker Siemens Healthcare
- Speaker SIRTeX Medical
- Speaker BTG
- Speaker Merit Medical
- Speaker & Consultant Surefire Medical