Emerging technology to improve cervical cancer screening for low-income communities
A recent article published in Biophysics Reviews highlights the shortcomings of pap smears for cervical cancer screening and describes how advances in nanotechnology and machine learning can remove subjectivity and the need for expensive lab equipment.
Low-income nations, or remote regions of wealthier nations, historically have a higher death rate from cervical cancer due to the inaccuracy of Pap smears and the sophisticated resources required to interpret the results. The authors of the review, based at Massachusetts General Hospital (MA, USA), highlight how this emerging technology can close the testing gap in these areas.
Pap smears were introduced in the 1940s and require high-quality laboratories, properly trained clinicians and pathologists as well as repeated screenings for an accurate result. These conditions are not widely available in many countries, particularly in lower-income countries or remote regions of wealthier countries.
“The Pap smear has done wonders in terms of reducing mortality from a cancer that is very treatable when caught early and almost invariably fatal when it is caught late,” explained Cesar Castro (Massachusetts General Hospital). “And it is not even a great test. Part of its imperfection is that there is subjectivity to it. The trained eye is the limiting step in the process. The untrained eye, or relatively untrained eye, can miss cancers.”
The subjectivity of the test is cited as the main limiting factor that has led to higher death rates from cervical cancer in lower-income countries. The authors suggest that advances in machine learning are the key to addressing this misinterpretation and would lead to a significantly higher accuracy.
Recent advances in nanotechnology have also been used to support these updates in machine learning and next-generation sequencing technologies. This includes adding HPV testing to the cervical cancer screen to more accurately predict the long-term likelihood of developing cervical cancer in light of any precancers.
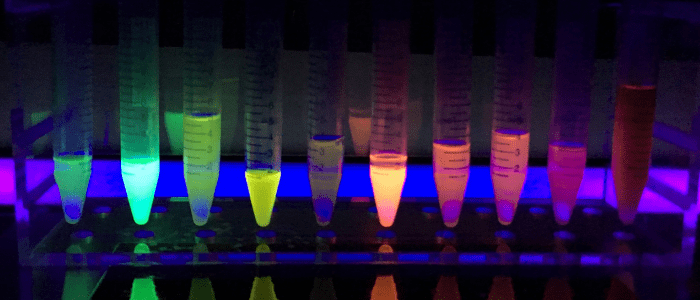
One technique involves screening with tiny beads made of biological material that form a diamond shape when they contact HPV. Those shapes can be detected with powerful microscopes. When those microscopes are not available, a mobile phone app, built through machine learning, can be used to read them.
“Similar to COVID-19 testing, we have great technology in places like the United States that does not work well enough in other countries,” explained author Hyungsoon Im(Massachusetts General Hospital and Harvard Medical School, MA, USA). “This is why there is great motivation to find next-generation, affordable technology to address this problem.”
Source: www.eurekalert.org/pub_releases/2021-03/aiop-cct032421.php



