Cancer Drugs Fund and CML: an unhappy alliance
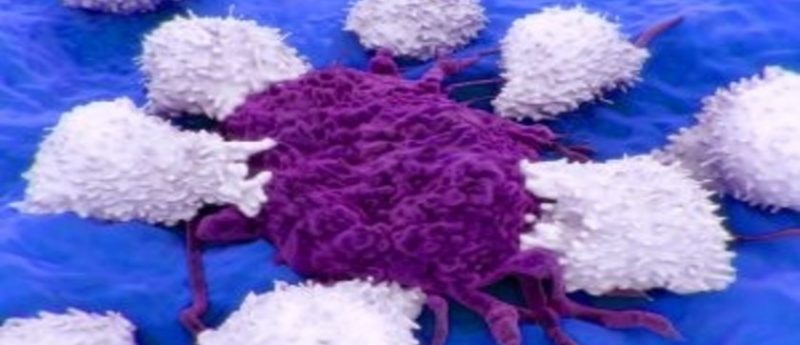
To call chronic myeloid leukemia (CML) the ‘poster child’ of cancer may seem to trivialize the devastating effects of a cancer diagnosis. The description does however succinctly reflect the outstanding improvement in the prognosis of CML since 2001, occasioned by the ability to target therapy once the causative genetic changes were understood.
Today, the majority of patients newly diagnosed with CML can expect a near normal life expectancy on one or more of five licensed drugs. Not however in England, where access to these agents has been increasingly limited by successive decisions from the Cancer Drugs Fund (CDF). Following recent CDF delistings, many English patients will now return to the prognosis of the 20th century, unlike their counterparts in the devolved nations.
The pathogenesis underlying CML is the presence of a fusion oncogene, BCR-ABL1, itself the product of the chromosomal translocation, t(9;22), the Philadelphia (Ph) chromosome [1]. BCR-ABL1 encodes a 210kD fusion protein termed Bcr-Abl1 – a dysregulated tyrosine kinase – involved in cellular proliferation, migration and apoptosis.
The clinical manifestation of Bcr-Abl1 is a triphasic disease. The initial chronic phase (CP) is characterized by an elevated white cell count, fatigue, night sweats, anorexia, weight loss and splenomegaly, which can be relieved (but not cured) using the oral agent hydroxycarbamide, or subcutaneous a-interferon (IFN). Using these drugs CML inevitably terminates in the blastic phase (BP), akin to an aggressive form of acute leukemia and virtually untreatable.
A period of instability in terms of loss of control of symptoms despite HC or IFN, usually precedes BP and is known as acceleration. Prior to the introduction of the class of drugs known as the tyrosine kinase inhibitors (TKI), the only curative therapy was allogeneic stem cell transplantation (allo-SCT), applicable to younger patients with fully matched donors. Since the median age of onset of CML is 60–65 years, the proportion of patients eligible for transplant (where transplant was readily available) was always less than 30% of the total population, and the associated transplant-related mortality meant that fewer than 15% survived long-term. Without transplant the median survival was 6–7 years [2].
Following the discovery of BCR-ABL1 in the early 1980s [3,4], some 15 years elapsed before the introduction into clinical practice of the first-generation TKI, imatinib. This once daily oral agent revolutionized the treatment and prognosis of CML [5]. From its first use in man in June 1998, imatinib moved rapidly through Phase I, II and III studies and was licensed initially for IFN failure and then in 2002 for front-line therapy.
Approximately half of the CML patients respond well and durably, but others fail through primary resistance, acquired resistance and/or intolerance to imatinib. Some resistant individuals had acquired single point mutations in the kinase domain (KD) of Bcr-Abl1, impairing binding to imatinib [6], a finding that led to the development of the second generation drugs, dasatinib, nilotinib and bosutinib, awarded marketing authorization in Europe in 2006, 2007 and 2013 respectively.
These agents were not only effective against certain mutations (and also in cases where the mechanism of resistance was unknown), but were often better tolerated than imatinib. The final KD mutation to induce resistance, T315I, was sensitive to the third-generation agent, ponatinib [7]. The ability to change the TKI until settling on an effective and well-tolerated drug results in >90% of patients achieving deep responses and returning to a normal life expectancy [8].
Not only has CML proven the power of targeted therapy, but it has also demonstrated the value of monitoring through molecular testing. BCR-ABL1 is readily detectable by a highly sensitive, reverse-transcriptase quantitative polymerase chain reaction assay that can reliably identify up to 5-log reductions in tumor load. As the TKIs are given by continuous oral daily dosing, tumor load reduces over time, but patients destined to respond optimally to any of the drugs will demonstrate one, two and three log reductions at 3, 6 and 12 months, respectively. By contrast lack of such responses identifies a group that contains patients at risk of early progression, but who might respond well to an alternative TKI. This finding led to the worldwide adoption of consensus guidelines, which recommend early switching of drugs in patients who fail to achieve these molecular milestones [9].
Imatinib, dasatinib and nilotinib are licensed for frontline use, with dasatinib and nilotinib inducing deep molecular responses more rapidly and in more patients than imatinib [10,11]. Dasatinib, nilotinib, bosutinib and ponatinib are licensed for second or subsequent line use for TKI failure and/or intolerance.
The choice of which drug to use frontline is somewhat controversial; some 30% of patients on imatinib fail to achieve the 3-month milestone compared with under 10% for nilotinib and dasatinib [10,11], and even lower for ponatinib [12]. The second- and third-generation drugs have a small but important incidence of more serious side effects such as pleural effusions (dasatinib), chronic diarrhea and hepatitis (bosutinib), poor diabetic control (nilotinib), and arterial thrombotic events (nilotinib and ponatinib).
Many elect to use imatinib frontline and reserve the more potent agents for imatinib failure or intolerance. The selection of second- and subsequent-line drugs depends on the sensitivity of any KD mutation, the spectrum of adverse events and the pre-existing comorbidities. With five available agents, most patients find an effective drug with tolerable side effects, but often ring the changes before settling on the final choice.
More potent drugs with limited need tend to come with a higher price tag. Only imatinib and nilotinib satisfied NICE appraisals and are available in the UK for first- (imatinib) or first- and second-line use (nilotinib) in CP. Access to the other TKI was made possible through the CDF. Because CDF consideration occurred at different times for each drug, because the drug costs varied considerably and most probably because of a lack of understanding of the place of each drug in modern management, decisions lacked coherency.
This led to some nonsensical cases of poor medical care, including a diabetic with ischemic heart disease who failed imatinib, having to take nilotinib, with access to dasatinib or bosutinib only if the almost inevitable adverse event occurred; a patient with imatinib resistance because of a dasatinib-sensitive but nilotinib-resistant mutation being forced to fail nilotinib before being allowed dasatinib. This was subsequently made worse by the withdrawal of dasatinib for imatinib or nilotinib resistance even in the presence of a dasatinib-sensitive mutation.
Patients with more advanced-phase disease fared even worse. Dasatinib, the only TKI to cross the blood–brain barrier, a valuable attribute in a disease in which the central nervous system is a sanctuary site, is not permitted through the CDF, leaving the least-potent agent imatinib as the only drug available for the most aggressive form of the disease.
In the most recent CDF iteration, access to TKIs in England has been further limited – for patients who fail imatinib, they will access nilotinib if they are intolerant or resistant, irrespective of comorbidities and KD mutations. If nilotinib proves ineffective, often predictably, no other drug is available: bosutinib can be used only in the presence of intolerance, ponatinib only if the T315I mutation is present and dasatinib is unavailable.
Patients who are resistant to front-line nilotinib have no second-line agent. The stark choices are those of allo-SCT, available only to a minority and with a 30–40% transplant-related mortality [13] or the drugs of the preTKI era, rendering a controllable disease, fatal. Across the borders into Wales and Scotland, dasatinib, bosutinib and ponatinib are all available according to their licensed indication, an inequity that cannot be justified or explained, and which renders the management of CML a postcode lottery.
The original objectives of the CDF were laudable [14], and included:
- Provision of maximum support to NHS patients
- Putting clinicians and cancer specialists at the heart of decision-making, consistent with the Government’s wider policy of empowering health professionals and enabling them to use their professional judgement about what is right for patients.
Together with patient representatives, the National Cancer Research Institute (NCRI) CML Working Party, who surely satisfy the definition of ‘cancer specialists’, have campaigned for a logical approach to CML treatment throughout the UK, allowing the choice of the most appropriate agent for an individual, and offering to provide advice regarding the drug choice and to record the outcome of patients receiving CDF-approved agents.
Patients and physicians are mindful of the cost of these drugs and the need to control expenditure, but recent decisions result in the most inappropriate use of money, namely the prescription of a drug destined to be ineffective, and the early use of allo-SCT with its inherent risk of mortality and long-term morbidity. These are not drugs that extend existence by months or weeks but treatments that provide many years of good-quality life. The CDF will shortly be replaced by another entity – we must hope that future decisions are taken in conjunction with the experts and can be justified to patients whose futures are at risk.
Disclosures
Honoraria and research funding from Ariad, Bristol Myers Squibb, Novartis and Pfizer
Acknowledgements
JFA would like to acknowledge the support of the NIHR-BRC of Imperial College Healthcare NHS Trust
References
- Nowell PC, Hungerford DA. A minute chromosome in chronic granulocytic leukaemia. Science 132, 1497–1501 (1960).
- Apperley JF. Chronic Myeloid Leukaemia. Lancet. 385, 1447–1459 (2015).
- Heisterkamp N, Stephenson JR, Groffen J et al. Localization of the c-ab1 oncogene adjacent to a translocation break point in chronic myelocytic leukaemia. Nature. 306, 239–242 (1983).
- Gale RP, Canaani E. An 8-kilobase abl RNA transcript in chronic myelogenous leukemia. Proc Natl Acad Sci USA. 81, 5648–5652 (1984).
- Druker BJ, Talpaz M, Resta DJ et al. Effi cacy and safety of a specifi c inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med. 344, 1031–1037 (2001).
- Gorre ME, Mohammed M, Ellwood K et al. Clinical resistance to STI-571 cancer therapy caused by BCR-ABL gene mutation or amplification. 293, 876–880 (2001).
- Cortes JE, Kantarjian H, Shah NP et al. Ponatinib in refractory Philadelphia chromosome-positive leukemias. N Engl J Med. 367, 2075–2088 (2012).
- Sasaki K, O’Brien S, Jabbour E et al. Relative survival in patients with chronic-phase chronic myeloid leukaemia in the tyrosine-kinase inhibitor era: analysis of patient data from six prospective clinical trials. The Lancet Haematology. 2 (5), e186–e193 (2015).
- Baccarani M, Deininger MW, Rosti , et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood. 122: 872–884 (2013).
- Hochhaus A, Shah NP, Cortes JE et al. Dasatinib versus imatinib (IM) in newly diagnosed chronic myeloid leukemia in chronic phase (CML-CP): DASISION 3-year follow-up. J Clin Oncol. 30, 232–238 (2012).
- Larson RA, Hochhaus A, Hughes TP et al. Nilotinib vs imatinib in patients with newly diagnosed Philadelphia chromosome-positive chronic myeloid leukemia in chronic phase: ENESTnd 3-year follow-up. Leukemia. 10, 2197–2203 (2012).
- Lipton JH, Chuah C, Guerci-Breslet A et al. Epic: A Phase 3 Trial of Ponatinib Compared with Imatinib in Patients with Newly Diagnosed Chronic Myeloid Leukemia in Chronic Phase (CP-CML). Blood, 2124(21), 519 (2014).
- Pavlu J, Szydlo R, Goldman JM, Apperley JF. Decades of transplantation for chronic myeloid leukemia: what have we learned? Blood. 117(3):755–763 (2011).
- The Cancer Drugs Fund – a consultation, 27 October 2010, Gateway reference 14909 http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Consultations/Liveconsultations/DH_120834
Author biography
Professor Jane Apperley qualified in Medicine from the University of Birmingham in 1979. After initial specialization in internal medicine she completed specialist training in hematology in Birmingham, London and Cambridge. During this time Professor Apperley spent 2 years as a postdoctoral fellow at the Children’s Hospital in Boston (MA, USA) where she received training in gene transfer and therapy.
She was appointed as Senior Lecturer and Honorary Consultant Physician to the Hammersmith Hospital in 1993 and was later promoted to Reader (2000) and then Professor of Haemato-oncology (2002). Her particular interests are the biology and management of chronic myeloid leukemia (CML) which has led naturally to an extensive experience in stem cell transplantation and more recently, to the use of signal transduction inhibitors in this disease. Professor Apperley also has a long-standing interest in the impact of hematological diseases and their treatment on fertility, pregnancy and fetal outcome.
Professor Apperley has been the Chief of Service for Clinical Haematology at the Imperial College Healthcare NHS Trust since 2003 and Chair of the Department of Haematology at the Imperial College since 2004. She is the past-President of the European Group for Blood and Marrow Transplantation (EBMT), JACIE and the British Society of Blood and Marrow Transplantation and servedd on the Advisory Board of the CIBMTR. She was one of the founders of the annual ESH-EBMT training course in stem cell transplantation, now in its 15th year. Currently she is an active member of the NCRI CML Working Party, serves as the stem cell transplant lead within the haematology working party of the London Cancer Alliance, and represents North-West London in the NHS England Stem Cell Transplant Clinical Reference Group. Her group cares for one of the largest cohorts of patients with CML in Europe and are active participants in clinical trials in CML.
Disclaimer
The opinions expressed in this opinion piece are those of the author and do not necessarily reflect the views of Oncology Central or Future Science Group.





