Research gives new hope to patients undergoing stem cell transplants
The Anthony Nolan Research Institute (ANRI, London, UK) has completed the biggest UK-wide study into the factors that can determine the success of a stem cell transplant.
The results, published recently in Journal of Bone Marrow Transplantation, ratify a trend that the age of the stem cell donor can directly affect patient outcomes, with younger donors leading to better survival rates for recipients. For the first time, the study also highlights that patients and matching donors carrying a common virus are able to compensate for a genetic mismatch.
Currently, donors are selected on the basis of their human leukocyte antigen (HLA) type and if it matches well with the patient – little is known as to whether patient survival is affected by other donor factors. ANRI’s latest research, however, provides the possibility to improve transplant success rates by identifying secondary factors that may play a role.
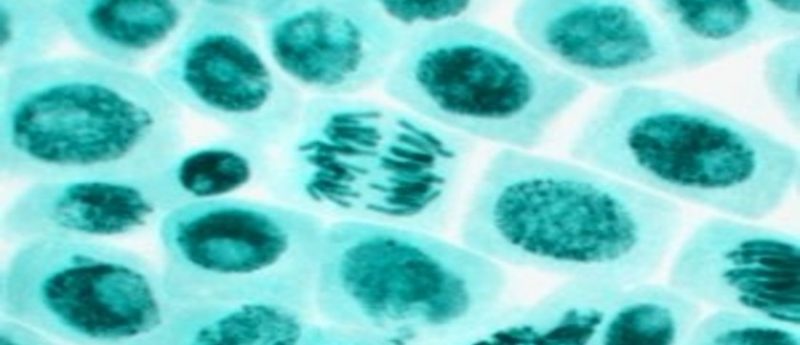
The study demonstrates that donors selected under the age of 30 resulted in patient survival rates of 45% compared to patients over 30, who resulted in a 38.6% survival rate. Anthony Nolan is the first UK stem cell register to reduce the age for joining to 16, as well as install an upper age limit of 30; other UK registers currently have an upper age limits of 45 and 55.
The researchers also made a ground-breaking discovery that matching the donor and patient cytomegalovirus (CMV) status may result in a significant improvement on patient survival. CMV is a common virus that affects 50-80% of the general population, and lies dormant in most healthy people. Patients undergoing transplant, however, have compromised immune systems, thus allowing the virus to reactivate. The team noted that a HLA mismatch could be compensated by matching for CMV; HLA-mismatched patients who did not have a CMV-matched donor were 1.5 less likely to survive than patients with a CMV match. This revelation could allow clinicians to improve survival rates for patients without a HLA-matched donor by matching the donor and patient CMV status.
Given these results, Anthony Nolan experts are exploring ways of typing donors for CMV when they join the stem cell donor register. This will allow CMV status to be included as a factor when transplant centers are selecting potential donors.
Lead author Steven Marsh (ANRI) commented: “This breakthrough will help us discover new and more effective ways to make sure patients in need of a transplant get the best possible match to cure blood cancer and blood disorders. The study confirms that younger donors lead to better transplant outcomes, and shows Anthony Nolan is leading the way by targeting 16-30 year olds to join the register.”
“Moreover, by establishing that CMV matching has a significant impact on patient outcomes, we are making it easier for transplant centres to make informed choices about the donors they select for their patients” Marsh concluded.
Source:
Shaw BE, Mayor NP, Szydlo RM et al. Recipient/donor HLA and CMV matching in recipients of T-cell-depleted unrelated donor haematopoietic cell transplants. Bone Marrow Transplant. 52, 717-725 (2017).