Study demonstrates why prostate cancer cells may develop resistance to treatment
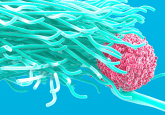
Researchers from the University of York (UK) have demonstrated that dexamethasone – a synthetic glucocorticoid hormone treatment routinely given to prostate cancer patients following radiotherapy – could potentially increase the resistance of cancerous cells, therefore increasing the possibility of cancer recurrence.
The study, recently published in Oncotarget, investigated potential novel biomarkers and targets that could be utilized to improve therapeutic strategies. The team observed that a potential biomarker candidate of radiation sensitivity was expressed in low levels by prostate cells after receiving glucocorticoid hormone supplements.
Lead author Norman Maitland (University of York) commented: “This was a really unexpected result of our investigation, so we took a slightly different direction in order to find out why these stem cells would become more resistant to cancer treatment.”
Within the study, the team identified the miR-99 family as potential biomarkers of radiation sensitivity and potential therapeutic targets to improve radiotherapy efficiency. This family of microRNAs has previously demonstrated an important role in the regulation of the DNA damage response via targeting of the SWI/SNF chromatin remodeling factors SMARCA5 and SMARCD1 in cell line models.
Owing to this, the team explored the cell populations of relatively radiation insensitive prostate cancer stem cells and cells in castration-resistant prostate cancer, which displayed low expression levels of miR-99a and miR-100.
Additionally, the team observed that treating cells with the synthetic glucocorticoid, dexamethasone resulted in decreased miR-99a and 100 expression, indicating a novel mechanism of miR-99a and miR-100 regulation in androgen-independent prostate cells.
“When more glucocorticoid hormones are ingested, the levels of MicroRNAs decrease even further, resulting in an increase in SMARCs. These SMARC proteins wind up chromosomes inside the cancer cells to make them resistant to treatment.”
The team then discerned that treating prostate cells with the glucocorticoid receptor inhibitor mifepristone sensitized prostate cells to radiation by increasing levels of miR-99a and miR-100 and decreasing expression of SMARCs, suggesting that the same dose of radiotherapy could kill more cancer stem cells when combined with glucocorticoid inhibitors.
“Hormone injections to counter the energy-sapping effects of radiotherapy and chemotherapy have been a standard part of after-care for 15 years or more, so we were surprised to find that the treatment was actually to the detriment of radiotherapy.”
Based on the initial findings of the study, the miR99 family could be identified as markers of radiation sensitivity and as potential therapeutic targets that could be utilized to improve the efficiency of radiotherapy.
Maitland concluded: “We now need to move into clinical trials to see whether blocking, rather than boosting, the glucocorticoids in patients could bolster the success rate of radiotherapy. It would ultimately mean that the patient is more tired after treatment, but there are other non-hormone treatments that could be used to improve energy levels that would not interfere with how we now believe stem cells to behave in cancer.”
Sources: Rane JK, Erb HHH, Nappo G et al. Inhibition of the glucocorticoid receptor results in an enhanced miR-99a/100-mediated radiation response in stem-like cells from human prostate cancers. Oncotarget. DOI: 10.18632/oncotarget.10207 (2016) (Epub ahead of print); University of York press release