NCRI 2018: Fluorescent marker helps improve accuracy of brain tumor cell removal
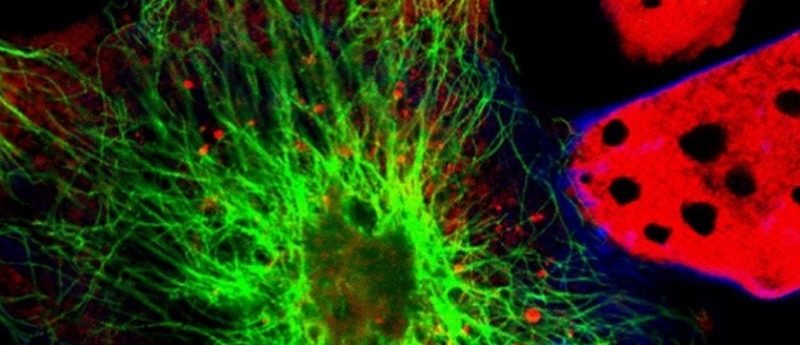
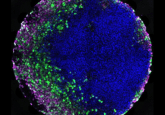
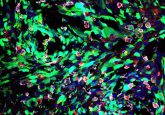
Researchers have found a new fluorescent biomarker that has the ability to distinguish high-grade glioma tissue from low-grade and normal brain tissue. This ability allows for the real time intra-operative differentiation of cell types during surgical procedures, resulting in a more accurate and complete removal of the tumor that can help improve outcomes.
The results are being presentedat the ongoing NCRI 2018 conference (4—6 November 2018, Glasgow , Scotland) by Kathreena Kurian from the University of Bristol (UK).
“Gliomas are difficult to treat with survival times often measured in months rather than years. Many patients are treated with surgery and the aim is to safely remove as much of the cancer as possible” explained Kurian.
“We wanted to see if using a fluorescent marker could help surgeons objectively identify high-grade tumour cells during surgery, allowing them to remove as much cancer as possible while leaving normal brain tissue intact,” Kurian added.
Researchers used 5-aminolevulinic acid (5-ALA) – a compound that glows pink when a light is shone on it. Previous research has shown that consuming 5-ALA results in its accumulation in fast growing cancer cells, allowing for it to be a potential fluorescent marker for high-grade glioma cells.
Participants of the study were provided a drink that contained the fluorescent compound before they underwent their procedure. During the surgery, operating microscopes were used to help surgeons search for fluorescent tissue and guide tumor removal. Removed tissue was analyzed the pathology lab in order to confirm the accuracy of the surgeons work from the cell type. In validating that the cells were high-grade glioma cells, further treatment could then be planed.
In a study across multiple hospitals, 99 patients in total were given the 5-ALA marker and were assessed for signs of fluorescence. During their operations, surgeons reported observing fluorescence in 85 patients, with 81 of these later confirmed by pathologists to have high-grade disease. One patient was found to have low-grade disease and three could not be assessed. In the 14 patients where surgeons did not observe any fluorescence, only seven tumors could be subsequently evaluated by pathology but in all these cases, low-grade disease was confirmed.
It should be noted that the study only included patients who were previously suspected to have high-grade tumors. A larger scale study with more patients who have the low-grade disease would be needed to provide more information on the technique.
Study leader Colin Watts (University of Birmigham) commented “Neurosurgeons need to be able to distinguish tumor tissue from other brain tissue, especially when the tumor contains fast-growing, high-grade cancer cells. This is the first prospective trial to show the benefits of using 5-ALA to improve the accuracy of diagnosing high-grade glioma during surgery.”
“These results show that the marker is very good at indicating the presence and location of high-grade cancer cells; the advantage of this technique is that it may highlight more quickly high-grade disease within a tumor during neurosurgery. What this means is that more of the tumor can be removed more safely and with fewer complications, and that’s better for the patient,” Watts continued.
The next steps for the researchers are to apply the 5-ALA technique to children with brain tumors and to assist in the differentiation of tumor tissue and scar tissue in patients with recurring brain cancer.
Sources: NCRI press release; WattsC, Jenkinson M, Ashkan K et al. Improving the intra-operative diagnosis of high-grade glioma using a fluorescence biomarker – A Progress Report of The GALA-BIDD Study. Neuro. Oncol. doi: 10.1093/neuonc/now188.034 (2018)